Background
The Accreditation Council for Graduate Medical Education (ACGME) states that residents must participate in quality improvement (QI) and patient safety (PS) initiatives during their training.1 In addition, as residents progress through their residency training and start to enter the workforce, they begin to learn about metrics related to quality of care provided and the patient’s experience while in the hospital. These metrics include the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS)2 scoring system and the Press Ganey3 which are publicly reported surveys of patients’ perspectives while in the hospital. Despite this, education in the QI and PS domain is scarce during medical school and many academic institutions may have a formal or informal quality improvement curriculum with significant variation.
At our institution, we recognized the need for formal and structured education in quality improvement and patient safety. We evaluated the activities in our residency program retrospectively to identify areas for improvement. Our curriculum did include conferences such as the morbidity and mortality conference, where residents learned about root cause analysis and subsequently reviewed a case with a focus on systems improvement and education. However, this was solely in a resident’s second year of training. Our goal was to incorporate education in these domains longitudinally throughout residency training.
Another one of our focuses when creating this curriculum was to have a collaborative approach to this education with the involvement of other team members within and outside of the department of medicine. With the growing focus on the importance of timely, accurate documentation in the medical record, we collaborated with the clinical documentation improvement (CDI) team to incorporate sessions where residents learned about the impact of documentation on billing and observed to expected mortality. We also included collaborative sessions with the infection control team, our quality coordinators and quality chief resident, and our nursing team to help foster relationships in the hospital. Through these initiatives, we devised “Rotation X”, a one-week long rotation with structured teaching in various facets of quality improvement.
Methods
Rotation X was created as both a collaborative and innovative one-week-long curriculum through which we provide targeted teaching for our learners across the continuum of their residency training. This is a mandatory rotation built into the schedule of every PGY-1 (intern) and PGY-3 (senior resident) in our internal medicine residency program. Every week, one PGY-1 and one PGY-3 are assigned to Rotation X and attend the sessions together to provide continuity and foster senior-intern collaboration.
At the beginning of Rotation X, each resident receives an email with the week’s schedule and calendar invitations to both the in-person and virtual sessions each day (Figure 1). Learners begin Rotation X with the CDI team at the beginning of the week. During this session, they review their documentation (such as patient care notes), focusing on billing diagnoses and observed versus expected mortality. The CDI team presents an overview of their workflow and how appropriate documentation of a patient’s clinical condition can alter mortality metrics. They then review patient admissions from the prior week done by the intern or senior resident and receive feedback on opportunities for improvement in documentation.
Learners are assigned a case to review, focusing on opportunities for improvement in patient care and learning about the process of completing a root cause analysis. This session provides a glimpse into a process that interns will further explore during their PGY-2 year when they present a morbidity and mortality conference. We have also introduced collaborative sessions with our pharmacy colleagues, focusing on medication reconciliation, and with the infection control team, with a focus on how to reduce catheter associated urinary tract infections (CAUTIs) and central line associated bloodstream infections (CLABSIs). This includes a pharmacy resident discussion on goal directed medical therapy, and a session on heart failure transitional care with the heart failure nursing team.
Furthermore, Rotation X includes close collaboration with the nursing team through the RN-MD communication series. During this session, four clinical scenarios are presented by the quality chief resident where better communication could have led to improved patient care. All members then have an open forum where residents and nursing staff discuss each other’s workflows and perspectives, improving communication going forward.
We end each week with a session titled “The Voice of the Patient,” where residents go to the bedside and visit with patients nearing discharge. This session is focused on understanding the factors that contribute to a patient’s experience while in the hospital, and the residents receive feedback from patients about this.
IRB exemption was obtained at our institution and both the PGY-1 and PGY-3 class were surveyed to ascertain their experience in the Rotation X curriculum. Survey questions included: the impact of CDI sessions on understanding O/E ratios, the voice of the patient session and appreciating the patient’s perspective, CLABSI/CAUTI rounds and understanding iatrogenic infection prevention, the RCA session and developing a root cause analysis, RN-MD sessions and demonstrating the importance of communication, as well as the CHF/pharmacy session and understanding role of goal directed medical therapy (PGY-3 only).
Results
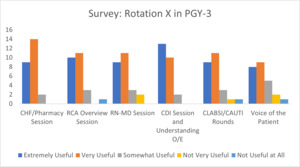
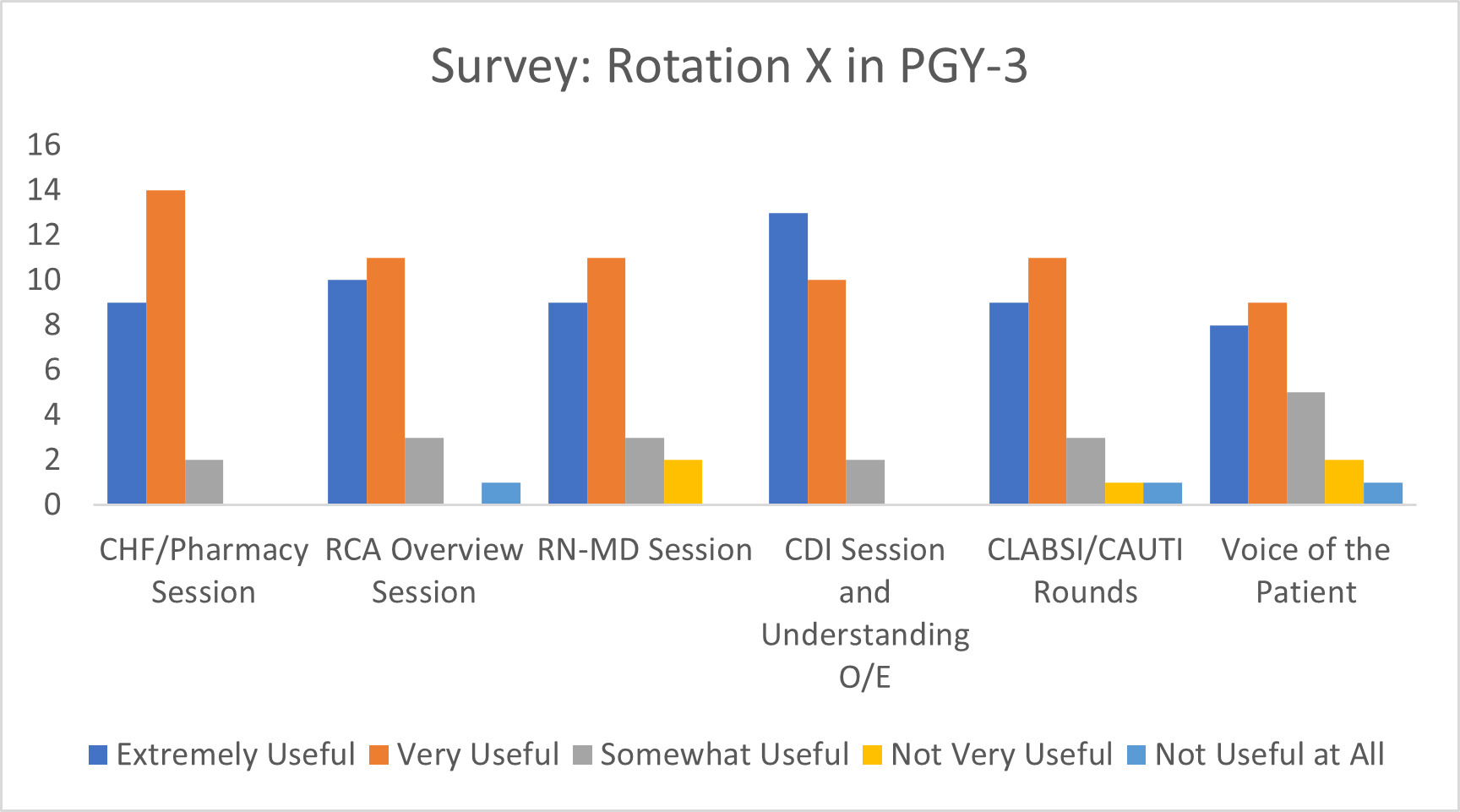
All residents participating in Rotation X were surveyed over the course of a year to ascertain their perspective on the rotation. Of the PGY-3 class surveyed, 100% found the CHF/Pharmacy sessions at least somewhat useful, with 96% for the RCA overview session, 92% for the RN-MD sessions, 100% for the CDI sessions, 92% for the CLABSI/CAUTI rounds, and 88% for the voice of the patient session. For these same sessions:92%, 84%, 80%, 92%. 80%, and 68% found these sessions either very or extremely useful, respectively.
We also surveyed our PGY-1 class to evaluate the effectiveness of this curriculum, with similar results. Of the PGY-1 residents, 77% found the RCA sessions at least somewhat useful, with 90.9% for the RN-MD sessions, 100% for the CDI sessions, 86.3% for the CLABSI/CAUTI rounds, and 90.9% for the voice of the patient session. Reviewing these sessions: 68%, 63.6%, 68%, 59%, and 50% believed these sessions were either very or extremely useful, respectively.
We also incorporated a session related to managing congestive heart failure in collaboration with the pharmacy and the heart failure nursing team, which 100% of participants found helpful in understanding the importance of guideline-directed medical therapy.
Discussion
With the growing landscape of quality improvement and patient safety in medicine, we sought to seamlessly integrate a focused curriculum into our internal medicine residency program. Through Rotation X, we created a weeklong rotation embedded with collaborative sessions curated to engage our learners in these domains.
Overall, we surveyed all participants who completed Rotation X and received resoundingly positive feedback from all post-graduate-year residents. In addition to the focus on QI and PS, we incorporated resident teaching sessions into the afternoon to help them grow as leaders, including dedicated bedside teaching sessions with medical students on their internal medicine rotation.
In particular, we found that both the RN-MD communication series and the voice of the patient session were particularly well received by our residents and nursing colleagues. The RN-MD communication series has provided an innovative forum for open discussion regarding scenarios in the hospital and now serves as a bridge between residents and nursing staff to help improve communication. We have engaged nursing staff from all medical and intensive care unit floors with a weekly rotating schedule to expand this collaboration further.
Residents found the voice of the patient session to be an eye-opening experience and a lens into the actual perspective of patients who are admitted to the hospital. Through this session, residents could engage with patients nearing discharge and genuinely focus on their unique experience in the hospital and how it could have been improved. This session will help our learners grow in the patient experience domain as they transition to the next career step.
Currently, resident satisfaction and perceived training benefit of Rotation X are limited to survey data, which consequently is subject to retrospective and responder bias. In the future, we plan to continue collecting survey data as the rotation is expanded to include a high-value care curriculum, as well as further input from multidisciplinary teams at our institution.
Conclusion
QI curricula for internal medicine residents are sparse in the literature. Fok and Wong et al. demonstrated improvement in resident education through a competency-based QI curriculum.4 In addition, Ogrinc et al. showed that integrating QI into the inpatient rotation for resident physicians led to improvement in educational metrics, and residents were satisfied with the curriculum.5 However, Rotation X is unique in that we present a dedicated weeklong curriculum tailored to QI and PS. Our curriculum is easily adaptable and can be integrated into existing programs. It can also be tailored to a program’s particular needs as sessions can be modified based on a program’s goals, and it also helps to promote collaboration within the hospital system.
Author Contributions
All authors have reviewed the final manuscript prior to submission. All the authors have contributed significantly to the manuscript, per the International Committee of Medical Journal Editors criteria of authorship.
-
Substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work; AND
-
Drafting the work or revising it critically for important intellectual content; AND
-
Final approval of the version to be published; AND
-
Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Disclosures/Conflicts of Interest
The authors declare they have no conflicts of interest.
Corresponding Author
Alexander Somerville MD
Department of Internal Medicine
SUNY Upstate Medical University
Email: alexgsomerville@gmail.com