Healthcare environments are becoming increasingly challenging, and the demands of the inpatient domain are exacting a substantial emotional toll, which is having negative repercussions. Emotional triggers in our environment, such as workplace toxicity, patient safety and traumatic events, work overload, and patient and family factors, continue to negatively impact patient care and the wellness of healthcare personnel. Due to this development, many healthcare staff have retired prematurely, moved to other disciplines, or reduced their work hours.1,2
The medical profession’s success in addressing many clinical conditions, notably cardiac diseases, cancer, metabolic disorders, and infections such as HIV and, more recently, COVID-19, has raised society’s expectations in terms of patient care outcomes. This has made the delivery and conveyance of any form of negative news challenging. Increasing demands for more interventions amid co-morbid conditions indicating medical futility have resulted in moral injury in the inpatient setting. In view of the oath to do no harm, and to take steps to ensure patients’ benefit, ethical dilemmas are being encountered with some of these demands for medical interventions. Easy access to online medical information, which may not be fully accurate or applicable to all patient care scenarios, has made discussions about appropriate medical decision-making challenging, as some patients/families raise anecdotal reports to support their requests. Additionally, in our fast-paced world, patients have been primed to receive information in the shortest possible time. Therefore, they do not take kindly to what they perceive to be delays in obtaining results of diagnostic procedures or responses to therapeutic interventions.3
The erosion of trust in the medical profession, through the concerted efforts of some individuals and, in some cases, self-inflicted, has positioned our views against those of some of our patients. The respect for patient autonomy in these cases adds to the moral injury faced in the inpatient domain. Amidst the issues of patients’/families’ expectations, easy access to online information, and erosion of trust in healthcare establishments, significant changes are taking place in the healthcare industry, which have been challenging for society to fully appreciate. Some of these include:
-
Regulatory changes regarding determinants of level of care in the inpatient setting, prior-authorization requirements for medications and procedures, and scenarios deemed appropriate for outpatient evaluation.
-
Segmentation in the spectrum of services available in various hospitals based on clinical factors or attempts to leverage economies of scale. Hospitals that are part of a larger system are increasing the segmentation of procedures and interventions to specific ones or referring patients to other systems.
-
Patients are sometimes unaware of restrictions posed by their selected insurance plans due to co-insurance, deductibles, and the adoption of tiered systems for patient referrals and medications prior to encounters in the inpatient domain.
How do we stay true to our professional values and stay motivated in this changing environment?
Much emphasis has been placed on individuals building their resilience through the adoption of self-compassion techniques, re-framing their frustrations, being flexible, and having enough physical and emotional rest. However, these personal competencies need to be buttressed by social competencies. The components of emotional intelligence provide a framework for us to navigate this new terrain successfully.4–7 Healthcare benefits of emotional intelligence include:
-
Improved communication and teamwork
-
Resilience and the ability to respond while under pressure
-
Increased empathy and empathetic bedside manners
-
Enhanced quality of patient care
-
Professional/career satisfaction
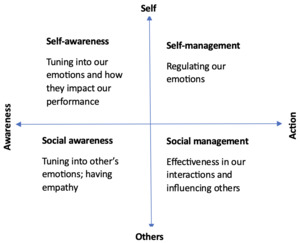
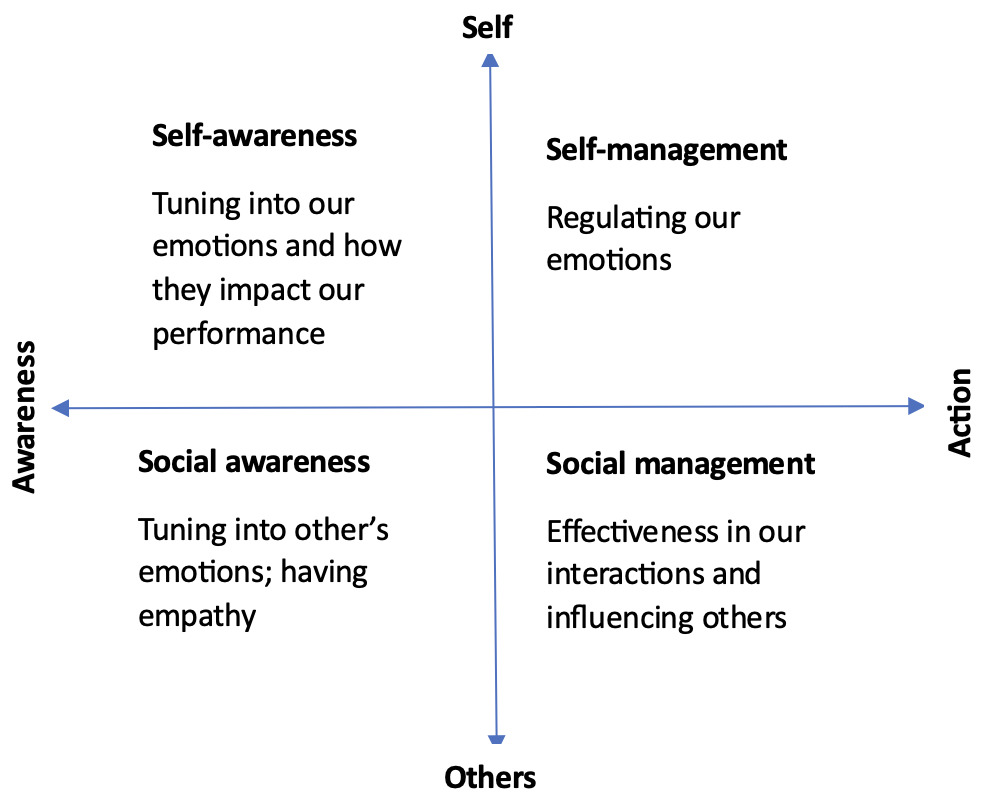
The major components of emotional intelligence (Figure 1) are8:
-
Self-awareness - Awareness of our emotions is not self-serving. It results in self-attention, care, and management, essential for effective service in our various roles.
-
Self-regulation - Awareness of the need to control the space between a trigger/stimulus and our responses helps us make better choices and enhances our adaptability and calmness under emotionally stressful circumstances.
-
Empathy – This helps us understand and respond to the needs of others appropriately.
-
Social skills – The ability to accurately perceive emotions in other people; the thoughts and feelings driving their behavior enable us to successfully manage relationships and/or conflict to attain desired goals.
We cannot control all the factors negatively affecting our work environment, but we can and should take care of ourselves. The emphasis on emotional intelligence is a much-needed resource for our success in our ever-changing environment.
Disclosures/Conflicts of Interest
The author has no conflicts of interest to disclose
Corresponding Author:
Kwame Dapaah-Afriyie, MD
Professor of Medicine, Clinical Educator
Warren Alpert Medical School at Brown University
Division Director
Division of Hospital Medicine
The Miriam Hospital, 164 Summit Avenue, Providence, RI 02906