Hospitalists serve as the foundational “brain architecture,” shaping medical students and residents through their teaching, patient care, and interactions with families and trainees. Teaching has consistently been identified as a significant contributors to job satisfaction by the hospitalists.1,2 Medical students and residents view hospitalists as effective teachers and enjoy being part of their teams.3,4 Hospitalists acting as inpatient teaching attendings contribute to reduce the length of stay and resource utilization while enhancing resident education.4
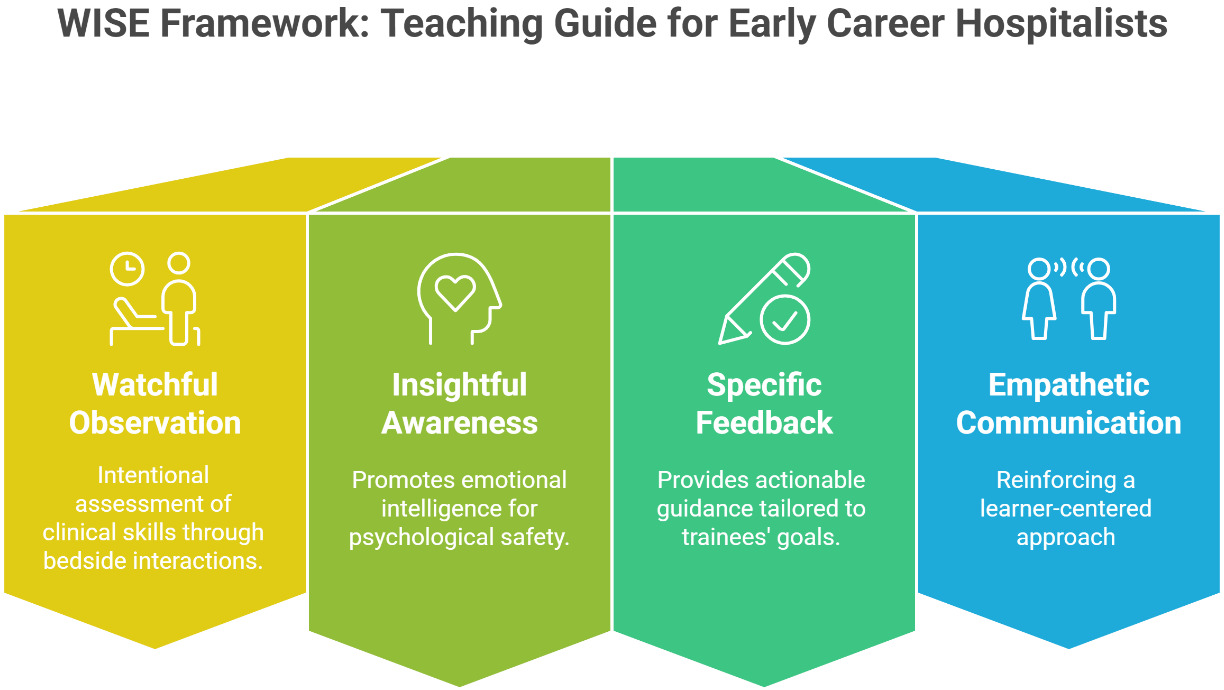
The proposed WISE framework encompassing Watchful Observation, Insightful Awareness, Specific Feedback, and Empathetic Communication offers hospital medicine educators a practical and effective tool to create the best possible, nurturing learning environment (Figure 1).
Watchful Observation
Attending physicians often struggle to provide effective feedback due to limited observation of trainees. To address this, establish a focused assessment and plan during pre-round discussions and encourage residents or interns to lead bedside rounds, presenting the previously discussed assessments and plans to patients and their families. A helpful tip is to guide trainees to share three major updates with the patient during bedside rounds. During on-call hours, observe trainees taking patient histories or performing exams, even briefly, and note their bedside manner, presentations, and clinical reasoning. Intentional observation enables meaningful and specific feedback on strengths and areas for improvement, helping trainees enhance their skills.
Insightful Awareness
Educators’ awareness is critically important as they set the tone for overall learning environments. Self-aware educators are mindful of their emotional triggers, biases, and strengths while working with trainees of different personalities and backgrounds.2,5 A brief self-reflection can sharpen self-awareness. For instance, after delivering a chalk-talk, spend two minutes identifying two or three aspects that were well-received by trainees and two or three areas that fell short of expectations. Our medical trainees are ethnically and culturally more diverse than before, underscoring the importance of cultural awareness for educators.2,6 For example, an international medical graduate (IMG) may not be fully aware of American idioms, slang terminology, and team-based learning approach. Hospitalist educators must foster a psychologically safe environment, demonstrate patience to promote culturally inclusive education.
Specific Feedback
Trainees need feedback to develop and refine their clinical skills. To better tailor feedback, asking trainees to share two or three goals or skills they are working to improve at the start of the rotation provides insight into their priorities and challenges, enabling meaningful feedback at the end of the rotation. Just as patient actions are documented, maintaining a record of trainees’ strengths and areas for improvement ensures the ability to provide detailed and constructive feedback. Before sharing feedback, encouraging trainees to reflect on two or three things they did well during the rotation and two or three areas needing improvement fosters self-assessment. Similarly, seeking trainees’ feedback on teaching and rounding styles enhances efficiency and impact. Exceptional attending physicians follow a key principle: address concerns privately and offer compliments publicly.
Empathetic Communication
Empathy is essential for hospitalists to be effective medical educators, as it helps them understand the values, goals, and challenges of trainees with diverse personalities.2,6 Every trainee is unique; some share input spontaneously, while others remain quiet until prompted. At the start of each rotation, a useful approach to help trainees feel included and valued is “biographic rounding.” In this practice, trainees and attendings share their names, educational backgrounds, and hobbies, serving as a cornerstone for engagement and breaking down barriers between them.2 Vulnerability is a superpower for trustworthy educators. Sharing your own learning challenges, such as struggling with acid-base disorders, along with effective strategies that helped you foster a safe and harmonious learning environment. Using trainees’ preferred names, ensuring correct pronunciation, and asking if you’re unsure fosters a sense of being seen, heard, valued, and included.
“Medical education is not just a program for building knowledge and skills in its recipients… it is also an experience which creates attitudes and expectations.”
- Abraham Flexner
Author Contribution
All Authors have reviewed the final manuscript prior to submission. All the authors have contributed significantly to the manuscript, per the ICJME criteria of authorship.
-
Substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work; AND
-
Drafting the work or revising it critically for important intellectual content; AND
-
Final approval of the version to be published; AND
-
Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved
Disclosures/Conflicts of Interest
The authors have no conflicts of interest to disclose.
Corresponding Author
Farzana Hoque, MD, MRCP, FACP, FRCP
Associate Professor, Department of Medicine,
Saint Louis University School of Medicine, USA
Email: farzanahoquemd@gmail.com
Phone: 314-257-8222