Background
Multiple sclerosis (MS) is a chronic, immune-mediated demyelinating disorder of the central nervous system. It predominantly affects women, with a female-to-male ratio estimated at 3:1 to 4:1.1 MS typically presents between the ages of 20 and 50 and manifests with a variety of neurological symptoms, including sensory disturbances, motor deficits, optic neuritis, and ataxia. These symptoms may occur in isolation or combination, often following a relapsing-remitting course.
The diagnosis of MS is based on the McDonald criteria (Table 1), which require evidence of dissemination of lesions in both time and space within the central nervous system.2 Dissemination in space (DIS) refers to lesions occurring in at least two characteristic CNS regions—periventricular, juxtacortical/cortical, infratentorial, and spinal cord—while dissemination in time (DIT) requires the presence of both enhancing and non-enhancing lesions on MRI, or new lesions on follow-up imaging, or the detection of CSF-specific oligoclonal bands. The 2017 revisions to the McDonald criteria allow for the diagnosis of MS following a single clinical attack if MRI and/or CSF findings go along with the criteria.
Applying the McDonald criteria in the clinical settings can present challenges. When a patient presents with only one clinically isolated syndrome and lacks radiological evidence of DIT, diagnosis may be delayed while awaiting additional clinical episodes or the results of CSF analysis. This waiting period may postpone the initiation of therapy, which is increasingly recognized as beneficial even in early disease stages.
Furthermore, spinal cord–dominant presentations of MS, such as syrinx often prompt a broad differential diagnosis. While spinal cord lesions are common in MS, isolated spinal cord symptoms in the presence of cortical or infratentorial lesions are relatively uncommon, as cortical involvement typically produces a broader constellation of clinical findings.3 This discrepancy can be challenging.
Case Presentation
A 43-year-old male with no significant past medical history presented with a 6-month history of progressively worsening paresthesia in the hands and feet. This was a single episode, and he denied any other neurologic symptoms in the past. His symptoms had rapidly ascended in level over a one-week period to the umbilical area, accompanied by numbness, decreased perineal sensation, and urinary difficulties. He reported gait instability and unintentional foot slamming due to numbness. He denied motor weakness, vision changes, headaches, or recent infections, except for a mild viral upper respiratory infection one month prior. There was no history of trauma, substance abuse, or family history of neurological conditions, but a maternal history of rheumatoid arthritis and an aunt with lupus were noted. On presentation, neurological examination revealed sensory deficits below the umbilical level, impaired proprioception in the lower extremities, and gait instability. Motor strength was preserved.
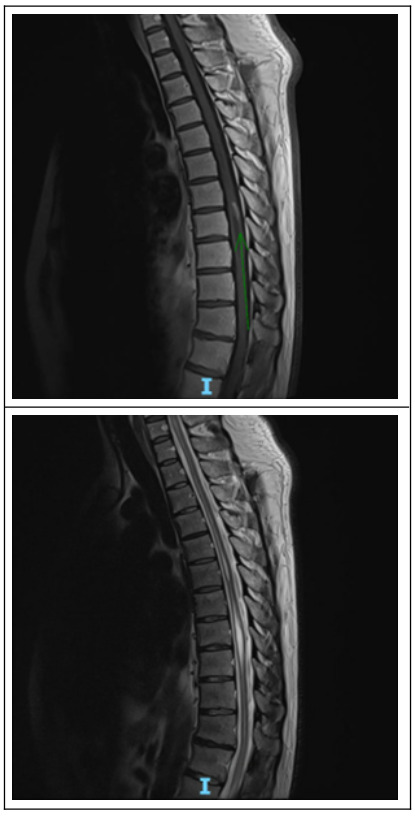
MRI of the brain showed scattered subcortical and periventricular FLAIR hyperintense lesions suggestive of demyelination. (Figure 1). Contrast-enhanced T1 did not show any lesions. Also, an MRI of the thoracic spine showed a syrinx from C5-T12 and patchy non-enhancing cervical cord signal changes with an intramedullary cord lesion at the level of T8 with linear enhancement. (Figure 2). An MRI of the brain revealed a few scattered subcortical and periventricular FLAIR hyperintense lesions as well as non-enhancing FLAIR hyperintense lesions in the anterior pontomedullary junction and left cerebellum. Laboratory workup revealed an elevated ESR, low methylmalonic acid, normal vitamin levels (B1, B6, B12, E), and negative infectious and autoimmune panels (e.g., ANA, dsDNA, viral studies). He was treated with high-dose intravenous methylprednisolone (250 mg every 6 hours for 5 days), gabapentin, and vitamin B12 supplementation. Ultimately, CSF analysis was positive for oligoclonal bands without cytologic abnormalities, confirming the diagnosis of MS. Neuromyelitis-optica gene and AQ4-IgG were negative. His neurological symptoms stabilized with therapy. Physical and occupational therapy were initiated, and the patient was discharged with outpatient neurology follow-up.
Discussion
This case underscores the diagnostic complexity of transverse myelitis within the context of demyelinating diseases like (MS). Maintaining a broad differential diagnosis is essential, necessitating the exclusion of potential etiologies such as infections and nutritional deficiencies. Particularly in male patients, even when symptoms do not exhibit the classic relapsing-remitting pattern, spinal lesions as part of MS should remain a consideration. Adherence to the McDonald criteria, which require evidence of dissemination in time and space, is instrumental in guiding accurate diagnosis, especially in atypical presentations.
In this patient, the presence of a syrinx—a fluid-filled cavity within the spinal cord—posed a diagnostic challenge. Syrinx formations are typically associated with conditions like syringomyelia or Chiari malformations and are relatively uncommon in MS patients.4 A case by Waziri et al.5 reported syrinx formations associated with demyelination.5 Weier et al.6 reported a prevalence of 4.5% of the syrinx in MS, highlighting their rarity.6 This reinforces the importance of not dismissing clinical suspicion of MS solely based on such atypical imaging findings.
Moreover, diagnosing MS after a single clinical episode presents additional challenges. The McDonald criteria allow for an MS diagnosis based on one clinical episode if MRI findings demonstrate dissemination in space and time. However, cases where patients present with a solitary episode and corresponding MRI findings are relatively rare. This case exemplifies such a scenario. Also, even with cortical FLAIR hyperintensities on MRI, his symptoms remained more related to spinal involvement, lacking visual changes or other cortical signs.7 It is also important to rule out infectious etiologies and autoimmune and nutritional deficiencies. This is a crucial step in directing the diagnosis, especially when waiting for laboratory workups, such as oligoclonal bands, that will take longer to produce results.
In conclusion, this case highlights the importance of considering MS in patients with atypical presentations, such as the presence of a syrinx or a single clinical episode. It underscores the importance for clinicians to follow appropriate rule-out processes and remain open-minded while applying diagnostic criteria to navigate complex cases effectively.
Author contribution
All Authors have reviewed the final manuscript prior to submission. All the authors have contributed significantly to the manuscript, per the ICJME criteria of authorship.
Substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work; AND
-
Drafting the work or revising it critically for important intellectual content; AND
-
Final approval of the version to be published; AND
-
Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Disclosures/Conflicts of Interest
The authors have no conflicts of interest to disclose.
Corresponding author:
Cinthia Reyes, MD
University of Miami at Holy Cross
4725 North Federal Highway, Fort Lauderdale, FL 33308
Phone: (954) 542-3257
Email: cyr22@miami.edu