An 86-year-old man with a greater than twenty-year history of rheumatoid factor (RF) and anti-citrullinated protein antibody (ACPA) positive erosive rheumatoid arthritis (RA), presented to the emergency department with gait instability and a mechanical ground-level fall. He had fallen on prior occasions due to severe bilateral joint deformities of his legs and feet. He was diagnosed with RA at age sixty-five and was started on methotrexate and infliximab. This was stopped after he developed a pulmonary aspergilloma. After a wedge resection of the lung lesion, he was prescribed etanercept monotherapy. This was eventually switched to golimumab because he was having difficulty with weekly self-injections. Golimumab was discontinued after two years due to a lack of efficacy and disease progression in the upper and lower extremities. A combination of sulfasalazine and tofacitinib was then tried, and he was eventually switched to tofacitinib monotherapy due to cytopenia. This regimen was discontinued after three years due to ongoing headaches and a dry cough. Eventually settling on a final regimen of hydroxychloroquine 200mg daily and methotrexate (MTX) at 12.5 mg every week. Episodes of epistaxis at higher MTX doses limited dose escalation. In addition, oral prednisone tapers for significant disease flares were prescribed.
The first lower extremity joint abnormality noted was bilateral hallux valgus deformity. This began at diagnosis and had progressed significantly by year five. Metatarsophalangeal (MTP) joint subluxation began later and affected the right foot more than the left. The second through fifth toes began crowding laterally later in his disease course and were associated with splaying of the forefoot seen on Xray. Hammer and claw toes developed after the first decade post-diagnosis and correlated closely with worsening pain, gait instability, and frequent falls. Surgical history included total right hip arthroplasty after a ground-level fall associated with a hip fracture four years ago. He had an elective right ankle fusion two years prior for right ankle instability and associated pain, which improved post-procedure. He reported good adherence to his medications, which included folic acid, hydroxychloroquine, and MTX. He had a 60 pack-year smoking history complicated by mixed interstitial lung disease (ILD) and chronic obstructive pulmonary disease (COPD) and was on chronic home oxygen therapy.
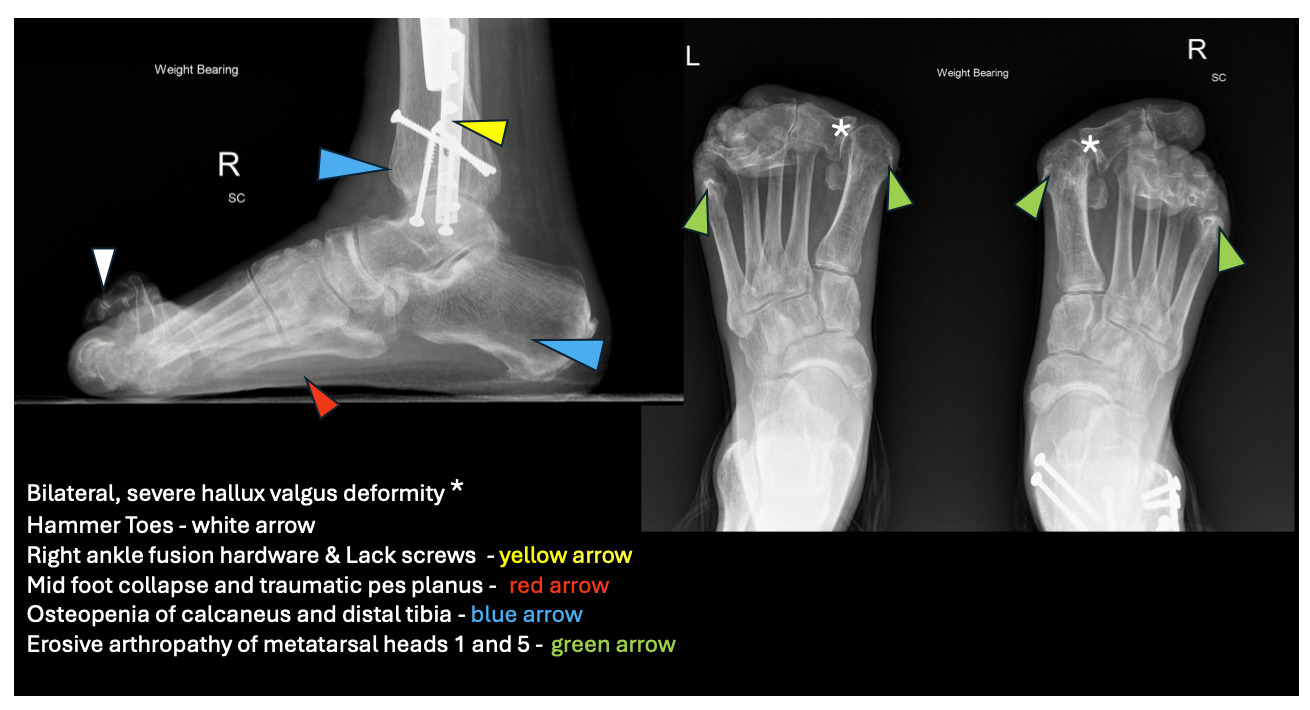
On exam, he had mild dyspnea and cachexia with bitemporal and extremity muscle wasting. His hands showed multiple chronic deformities, including wrist fusion, elbow flexion contractures, Z-shaped thumbs, and swan neck deformities. His feet showed bilateral, severe hallux valgus and multiple hammertoe and claw toe deformities. Weight-bearing radiographs of his feet (Figure 2) and legs confirmed bilateral hallux valgus, moderate bilateral first metatarsophalangeal osteoarthritis, and erosive irregularities of the first and fifth metatarsal heads concerning for erosive rheumatoid arthropathy. Diffuse bony demineralization and bilateral hammertoes were present. A right tibial intramedullary rod and right lateral distal fibular plate with Lack screws in the distal tibia and fibula, consistent with right ankle fusion, was noted.
Our patient did not tolerate multiple targeted biologic disease-modifying antirheumatic drugs (DMARDs) due to clinically significant side effects. Despite regular follow-up and early diagnosis, we were unable to prevent the progression of his disease. Subsequently, he was managed with hydroxychloroquine, MTX, and short courses of prednisone as the only pharmacologic therapy for his RA. In addition, his progressive decline is attributed to having the most severe form of rheumatoid arthritis. The co-occurrence of positive anti-citrullinated protein antibody (ACPA) and rheumatoid factor (RF) or “Dual antibody positive RA” is associated with a more severe form of the disease.1 This includes rapid advancement of joint inflammation, progression of radiographic changes, higher likelihood of extra-articular manifestations as well as severe ankle and foot joint deformities. While most RA patients will eventually develop foot and ankle involvement, early foot and ankle RA portends a more severe disease activity and is an independent risk factor for inability to attain remission.2,3
Genetic predisposition and toxins, such as cigarette smoke, activate an autoimmune response that results in anti-citrullinated protein antibodies and other pro-inflammatory cytokines, leading to immune activation directed at synovial tissue. Initial manifestations are symmetric, stiff, swollen, and painful joints, worse on awakening. As synovial inflammation worsens, the forefoot is usually the first lower extremity area affected. The progression of lower extremity disease occurred from the forefoot, midfoot, and eventually to the hindfoot. The first MTP joints develop painful, progressive bunions, called hallux valgus deformity. Progressive inflammation and ligament destruction of the metatarsophalangeal (MTP) joints result in characteristic subluxation. Toes dislocate upwards at the ball of the foot, pushing the metatarsal heads downward and creating painful calluses (Figure 1). The upward curling of the phalanges creates claw and hammer toes. Ligament weakening eventually causes midfoot collapse and pes planus. Hindfoot deformities manifest as ankle instability and pain. Surgical arthrodesis (Figure 2) is often associated with pain relief and improved mobility.4
Disclosures/Conflicts of Interest
None
Corresponding author
Michael E. Lazarus, MD
Professor of Clinical Medicine
757 Westwood Plaza, Suite 7501C,
Los Angeles, CA 90095
Email: MLazarus@mednet.ucla.edu
Phone: 310-597-0944