Introduction
Rapid (occurring within seven days of discharge) readmissions to the hospital are associated with significant morbidity and mortality.1 Unplanned 30-day readmission to a hospital in the United States is common with readmission rates ranging between 14-20% depending on discharge diagnosis, patient age and other factors.2 Factors associated with 30-day readmissions have been extensively evaluated in the literature whereas 7-day readmissions are less commonly examined.3,4 A readmission occurring within seven days of discharge may be presumed to be directly related to inpatient care. Still, factors associated with rapid readmission to the hospital have not been fully elucidated. Early or rapid readmissions may be more closely related to modifiable risk factors during the index admission. Identifying sources of risk for rapid readmission may allow for focused interventions to prevent readmission.
Known reasons for rapid readmissions are broad and may be related to the severity of the underlying disease process during index admission, socio-economic factors, comorbid conditions, errors in provider diagnostic and/or treatment approach among others.4 In phase one of this quality improvement initiative, we sought to identify reasons for rapid readmission for patients discharged from a general medicine inpatient service. Our main aim was to determine the frequency and severity of provider error, as this was deemed the most accessible modifiable risk factor for a hospital medicine practice.
Methods
Patients discharged from the inpatient medical service at The Miriam Hospital (Providence, RI) from October 2018 to February 2019 were identified. The Miriam Hospital is a 250-bed acute care hospital in Providence, RI and is part of the Lifespan Corporation health care system. There were a total of 6,245 discharges from the general medical service, approximately 40 discharges per day. One thousand four hundred readmissions (22%) occurred within 30-days of discharge, and 457 readmissions (7%) occurred within seven days of discharge. Patients discharged from the emergency room without being admitted, discharged from surgical services, and other non-medical services were not included. A readmission was defined as an admission to the hospital occurring within seven calendar days of hospital discharge. Medical records of patients readmitted within seven days of this timeframe were manually examined by Hospital Medicine providers on the Readmissions Quality Improvement Initiative Task Force. Providers reviewed admission notes, discharge summaries, and other pertinent data for the index and the subsequent readmission. Reasons leading to each readmission were identified and classified into one or more of 10 categories:
-
Subspecialty Care
-
Medications
-
Outpatient Follow Up
-
Clinical Judgement
-
High Hospital Utilizer
-
Severity of Disease/Failure to Respond to Treatment
-
Non-adherence/Discharged Against Medical Advice
-
Substance Use Disorder/Uncontrolled Psychiatric Disorder
-
Disposition
-
Other (unrelated)
Reviewers were provided with criteria and examples for the categorization of readmissions. See Appendix 1 for category definitions and case examples. In total, 371 charts were reviewed by seven hospitalist physicians. Reviewers were also asked to identify specific cases of provider error, if present, to highlight underlying issues which could be shared with the entire inpatient hospitalist practice. Readmission cases marked as related to clinical judgement error were re-reviewed by a second physician and abstracted.
Results
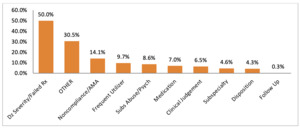
Three hundred seventy-one charts were reviewed. 50% of7-day readmissions were related to the severity of disease and/or lack of response to appropriate treatment. 30.5% of readmissions were related to causes falling outside the identified categories. Adherence challenges, patients with known high hospital utilization, and substance use disorder/uncontrolled psychiatric conditions accounted for 32.4% of 7-day readmissions. Readmissions related to clinical judgement accounted for 6.5% of the total readmissions. See Figure 1 for complete results.
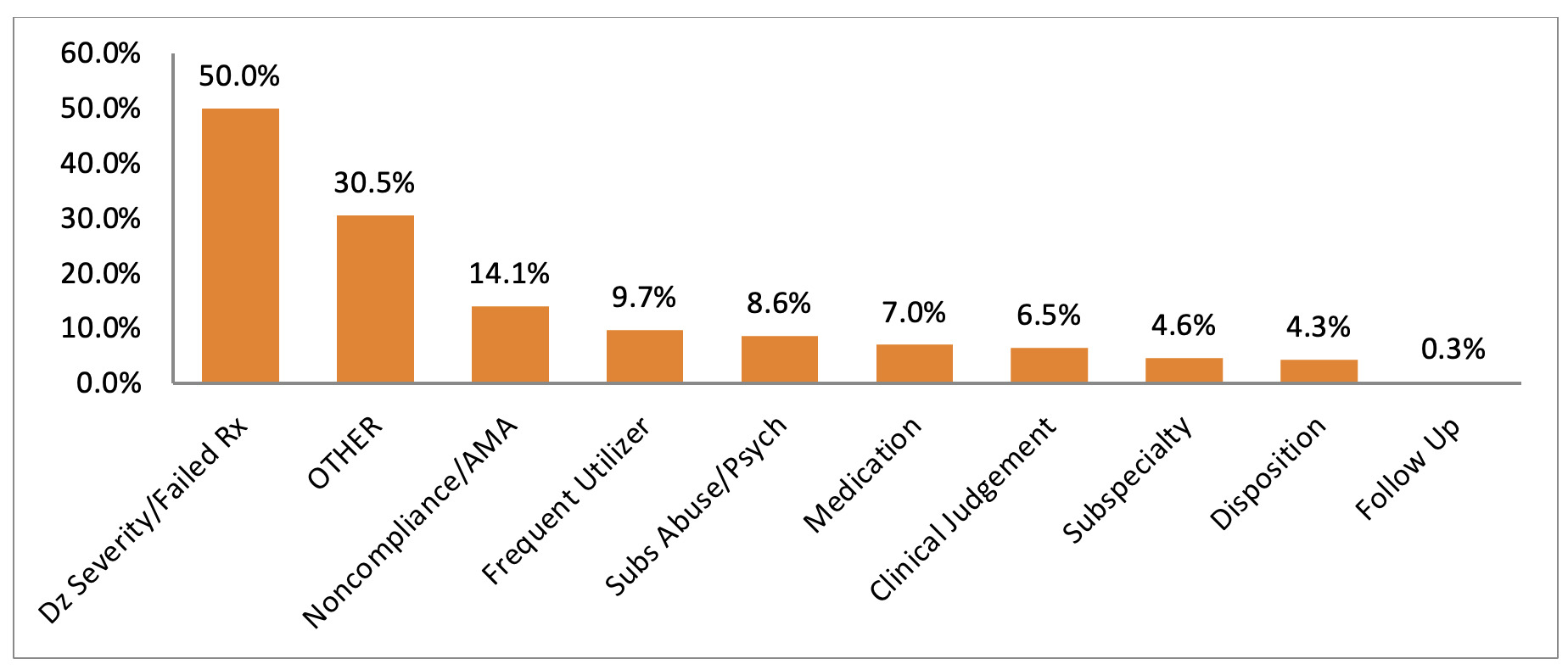
67% of the readmissions were associated with one category, 28% of the readmissions were associated with two categories, and 5% of the readmissions were associated with three-plus categories (Figure 2). Twenty-four cases were identified as being related to errors in clinical judgement. Diagnostic errors comprised 6 out of 24 cases and involved stroke (1), spinal cord disease (1), missed culture results (1), abdominal abscess (1), biliary disease (1) and Clostridium difficile infection (1). Treatment errors comprised 16 out of 24 cases and included incorrect or missing antibiotic treatment (9), inappropriate or missing medication treatment (3), failure to assess mobility (2), and others (2). Two cases did not fall under diagnosis or treatment errors.
Discussion
Rapid readmissions to the hospital, occurring within seven days of discharge, are an important area of examination for inpatient providers. Due to their temporal relationship to the index stay, 7-day readmissions may be more preventable than 30-day readmissions.5,6 Risk factors for 7-day readmissions are not well elucidated but may include the presence of certain chronic medical conditions such as chronic obstructive pulmonary disease, congestive heart failure, medication issues and others.7,8 Reducing 7-day readmissions is a primary goal for inpatient practices to reduce morbidity and mortality associated with repeat hospitalizations. Our results indicate that the majority of 7-day readmissions were attributed to the severity of the underlying condition during the index admission or a lack of response to appropriate treatment. We found that rates of rapid readmission related to diagnostic or therapeutic error were low, 6.5%, in our sample. Notably, 30% of early readmissions were not related to the reason for the index admission. 14% were related to nonadherence to treatment and patients who left the hospital against medical advice. Another 10% were related to the high utilizer population known to the hospital’s high utilizer committee, a complex subpopulation of patients with frequent visitation to the hospital. Inability to obtain medications and other medication-related side effects accounted for 7% of readmissions and another 9% were related to substance use and psychiatric disorders.
The vast majority of readmissions are related to disease severity, treatment adherence, substance abuse, and high utilization patients, which accounted for 82% of 7-day readmissions to our service. Improving outcomes in this heterogeneous population of patients and diagnoses remains a challenge.9,10
Clinical judgment errors were implicated in approximately 6-7% of cases. The most common errors were therapeutic and likely to involve incorrect or missing antibiotic therapy. Clinical judgment errors were reviewed, and common patterns emerged, including diabetes management, interactions between the anticoagulant, coumadin, antibiotics, and neurological symptoms in patients readmitted with stroke. Patients who were deconditioned and required physical therapy evaluation but did not receive an assessment were also found.
Based on the study results, five recommendations made to the inpatient providers included:
-
Review of insulin dosing at time of discharge
-
Review of coumadin and antibiotic medication interactions
-
Appropriately evaluate concerning neurological symptoms
-
Review antibiotic treatments and pending microbiological culture results
-
Mobility assessments should be performed for patients at risk of falls
There were several limitations to our quality improvement analysis that must be noted. This analysis was performed by providers from the hospital practice that was being evaluated. Providers on the quality improvement task force may have been reluctant to assign provider error to readmissions of patients that they may have cared for themselves or were seen by their colleagues. To mitigate this, providers were advised not to evaluate cases in which they were directly involved with the patient’s care. Hospitalist providers volunteered for the quality improvement initiative and were motivated to find areas for improvement in the medical record. Additionally, this initiative took place before the onset of the COVID-19 pandemic, which has significantly altered the care processes both in the hospital and in the outpatient setting.
Conclusions
Rapid readmissions to hospitals are frequently associated with severe underlying diseases. Readmissions due to clinical judgement errors represent a small proportion of rapid readmissions. To address commonly encountered clinical errors, inpatient clinicians should carefully review diagnosed infections, culture data, and antibiotics at the time of discharge, as well as the use of insulin, and the anticoagulant, coumadin which has a high potential for interaction with other medications.
Acknowledgements
Amer Alsamman, MD; Karl Herman, MD; Nabila Mazumder, MD; Abdelmoniem Moustafa, MD; Young Song, MD
Conflicts of Interest
The authors have no conflicts of interest to disclose.
CORRESPONDING AUTHOR
Arkadiy Finn, MD
Assistant Professor of Medicine, Clinician Educator
Warren Alpert School of Medicine at Brown University
Division of Hospital Medicine
The Miriam Hospital, Providence, RI 02906, United States of America
Tel: 401-793-2104
Fax: 401-793-4047
Email: afinn1@lifespan.org
ORCID: 0000-0002-1630-1137