Case Presentation
A woman in her 30s without known medical conditions presented after experiencing a fall and numbness and weakness of her lower extremities. The patient reported that approximately three weeks prior to presentation, she developed abdominal bloating and pain and was prescribed oral sucralfate for a presumed diagnosis of gastritis. At the same time, she began experiencing fingertip and toe “pins-and-needles” sensation that gradually progressed to include both hands and lower extremities up to the level of her bilateral buttocks. Over the previous two days she developed peri-oral numbness and reported being unable to feel her lips or tongue. These sensations were constant and patient denied any aggravating or alleviating factors.
On the day of presentation, she fell upon standing up from a sitting position as she could not support her own weight. She reported difficulty climbing stairs for the prior week and with rising from a seated position without the assistance of a railing or handle. She reported that due to the weakness she felt unsteady while walking.
Over the prior 3-4 weeks she reported a "poor diet, "consisting only of canned soups since the onset of her abdominal symptoms.
She has no previously diagnosed conditions, no prior surgeries, and her only medication was sucralfate 1 g four times per day. She denied use of over-the-counter medications and supplement and herbal medication use. She lived with her spouse and son and worked in an office environment. She reported a history of lymphoma in a close relative. She denied tobacco use and reported consuming 4-5 alcoholic beverages per week. She denied recreational drug use. At her baseline she performed all activities of daily living independently.
On review of systems, she denied fever, chills, change in appetite, fatigue, and night sweats, head injuries, hearing loss, tinnitus, loss of smell, chest pain, dyspnea on exertion, change in bowel habits, muscle aches, joint pain, headache, dizziness, syncope, memory problems, seizures, polyuria, polydipsia and heat or cold intolerance. She endorsed nausea, vomiting, abdominal pain and bloating.
Upon physical examination, temperature was 97.6 ℉, heart rate 83 beats per minute, respiration rate 18 per minute, blood pressure was 169/90 mmHg, oxygen saturation of 100% while breathing ambient air. The patient was well-appearing without evidence of distress. Oral and ophthalmic mucous membranes appeared moist and cervical lymphadenopathy was absent. Cardiac and pulmonary examinations were unremarkable. Abdominal examination revealed a soft, non-tender abdomen with normal bowel sounds. There were no rashes. A detailed neurological examination was performed:
Mental Status
Awake, alert, attentive and oriented to person, place, time and situation, fund of knowledge normal.
Language
Fluent without dysarthria, named 3/3 objects correctly, repetition intact.
Cranial Nerves
Visual fields full to confrontation, pupils equal and reactive to light bilaterally, extra-ocular movements intact, perioral numbness, temporomandibular joint and masseter strength 5/5 bilaterally, facial strength symmetric with normal eye closure and smile, hearing intact bilaterally, palate elevation symmetric, tongue midline.
Motor
Normal tone, normal bulk, no pronator drift noted.
Sensory
Diminished sensation to light touch in bilateral hands (entire hand) and in bilateral lower extremity throughout. Diminished sensation to pinprick to 60% in proximal upper extremity bilaterally, 40% in bilateral hands, and 40% in bilateral lower extremity including bilateral buttock. Diminished sensation to temperature in bilateral hands and bilateral lower extremity throughout, intact in proximal upper extremity bilaterally. Intact sensation to vibration and proprioception throughout.
Reflexes
Cerebellar
Intact rapid alternating movement bilaterally, intact finger to nose bilaterally, intact, intact finger tapping bilaterally.
Gait
Unsteady with normal steps, base, arm swing and turning, walking on heels unsteady but able to take a few steps, walking on toes unsteady but able to take a few steps, unable to tandem walk.
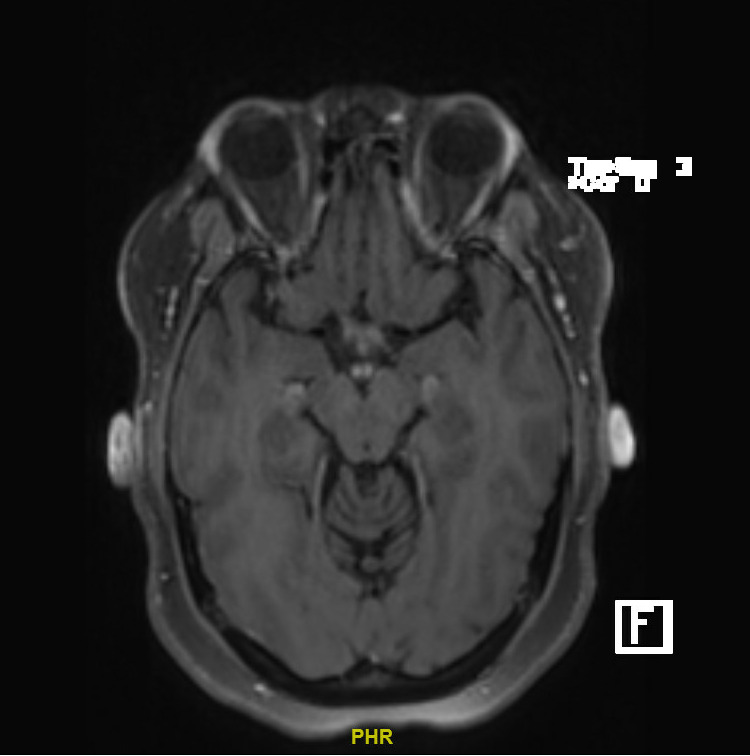
See Table 1 and Figure 1 for laboratory and imaging findings respectively.
Warren Alpert Medical School Student Presentations
Student (The Miriam Hospital)
Working Diagnosis: Acute Intermittent Porphyria
The patient presented with hypertension, hypokalemia, and hypomagnesemia, while endorsing symptoms of abdominal pain, nausea, and intractable vomiting, as well as bilateral ascending sensory neuropathy with subsequent weakness.
The patient’s constellation of nonspecific gastrointestinal (GI) and neurological symptoms, in addition to her hypomagnesemia and hypertension, was concerning for acute intermittent porphyria (AIP). This condition is caused by deficiency of porphobilinogen deaminase and can be triggered by poor diet and alcohol consumption, both of which were endorsed by the patient.
While patient lacked the classic presentation of red-purple urine, this finding is not essential for diagnosis. Differential diagnosis included electrolyte derangements secondary to hyperemesis gravidarum, celiac disease, dry beriberi due to thiamine deficiency, and Guillain-Barré syndrome (GBS). Workup would include a spot urine sample for heme precursor levels. I would also replete her electrolytes, order celiac serology and a pregnancy test, and begin low-risk thiamine supplementation. GBS workup would be held pending preliminary testing results.
Student (Rhode Island Hospital)
Working Diagnosis: Dry Beriberi
This patient’s findings are most consistent with a diagnosis of thiamine deficiency secondary to celiac disease. The mammillary body enhancement seen on magnetic resonance imaging (MRI) is a key diagnostic finding of thiamine deficiency. Additionally, this patient’s nausea and vomiting, distal paresthesias, ascending muscle weakness, and gait ataxia are common sequelae of thiamine deficiency. Although manifestations of thiamine deficiency vary, the absence of oculomotor dysfunction, nystagmus, and encephalopathy are more consistent with dry beriberi than Wernicke’s encephalopathy. The constellation of lab derangements indicates this patient has additional protein and vitamin deficiencies, leading me to believe this patient has an underlying malabsorptive disorder, likely celiac disease. This is also consistent with her gastrointestinal symptoms and weight loss. My workup would include serum and urine thiamine levels, as well as serum B6, B12, folate, zinc, vitamin D, and iron levels. I would also initiate a workup for celiac including a serum tissue transglutaminase IgA level and total IgA level. If the serology is positive, I would confirm the diagnosis via duodenal biopsy.
Student (Kent County Hospital)
Working Diagnosis: Acute Inflammatory Demyelinating Polyneuropathy/Guillain-Barré Syndrome
The patient’s reported history and physical exam findings of an antecedent GI illness, progressively ascending symmetric distal leg muscle weakness, hyporeflexia in lower extremity deep tendons, paresthesias and diminished sensation affecting distal extremities, back pain, dysautonomia as seen with patient’s hypertension and possible intestinal dysfunction, and perioral/intraoral numbness aligns with the features of GBS. Acute inflammatory demyelinating polyneuropathy (AIDP) is said to have clinical features such as autonomic neuropathy, ascending paralysis, cranial nerve defects, and pain that make this subtype more likely. Supporting laboratory values include normal white blood cell count and elevated alanine transaminase. Hypokalemia and hypomagnesemia can be attributed to GI losses; however, the lack of hyponatremia and hypochloremia indicate the etiology of these lab values is likely multifaceted and may be related to decreased oral intake in the preceding weeks. Confirmatory findings may include albumin-cytologic dissociation on cerebrospinal fluid analysis, signs of denervation and the presence of pathologic spontaneous activity on electromyelography.
Student (Veterans Affairs Medical Center, Providence, RI)
Working Diagnosis: Primary Hyperaldosteronism
The working diagnosis for this patient with paresthesias, GI symptoms, hypertension, hypokalemia and diminished strength and sensation is most concerning for primary hyperaldosteronism (PH). Less likely diagnoses include thyrotoxic paralysis, vitamin B12 deficiency and acute intermittent porphyria. The presentation of PH can often be non-specific, but commonly presents as hypertension with hypokalemia due to increased renal sodium reabsorption and potassium excretion, as seen in this patient. This patient’s neurological symptoms including muscle weakness, paresthesias, and hyporeflexia are likely secondary to hypokalemia causing potential difference derangements across nerve cell membranes. The GI symptoms are likely a result of hypokalemia-induced GI dysmotility. While the lack of metabolic alkalosis seen in this patient’s normal bicarbonate level may argue against PH, prior studies have demonstrated that roughly one third of patients with PH may have normal bicarbonate levels. Workup would include a plasma aldosterone to renin ratio and a 24-hour urine aldosterone level.
Dr. Daniel Mandel – Radiology Review
Post contrast MRI brain sequence revealed bilateral mamillary body gadolinium enhancement. Gadolinium enhancement reflects disruption of the blood-brain barrier. There is no evidence of involvement of other brain structures. This finding is classically associated with Wernicke’s encephalopathy, a condition arising from thiamine deficiency and is detected in 40-50% of cases. It may be accompanied by changes on MRI in the periaqueductal gray matter and thalamic nuclei which are not seen here. Isolated changes to the mammillary bodies are unusual.
Dr. Alexander Diaz de Villalvilla
We have a young woman who is presenting with falls, numbness and weakness for three weeks but we should be mindful that her pre-morbid health should be investigated as that may contain clues toward the current presentation. I note she reports a diet low in vegetables, meat and fruits as well as gastrointestinal symptoms. This appears to be a predominantly a primary sensory neuropathic issue presenting at the same time as bloating abdominal pain. The perioral numbness might make you think of hypocalcemia. We would to assess the patient’s proximal muscle strength by having her rise to standing from a sitting position. My differential is broad and includes syphilis, transverse myelitis, alcoholic gastritis, acute intermittent porphyria. Dry beriberi is high on my differential, due to its initial presentation involving peripheral nerve manifestations and eventually progressing into central nervous system symptoms also known as Wernicke’s encephalopathy. I would begin thiamine repletion, and test serum thiamine levels while ruling out the conditions listed earlier.
Hospital Course
Immune mediated polyneuropathy and thiamine deficiency were highest on the clinical team’s list of differentials. The patient was started on high dose thiamine repletion and received intravenous immunoglobulin and experienced improvement in her symptoms. Serum thiamine level returned undetectably low and as well as low serum pyridoxine (Vitamin B6) levels. Repletion with pyridoxine was dded and the patient was discharged in improving condition.
Discussion
Thiamine (Vitamin B1) deficiency is the cause of two major conditions: beriberi and Wernicke-Korsakoff syndrome. Patients at risk for these diseases include those with severe alcohol use, prior bariatric surgery, eating disorders, inflammatory bowel disease, end-stage renal disease, use of parenteral nutrition, or lack of access to thiamine-rich foods.1,2
In “dry” beriberi, patients have symmetrical peripheral neuropathy with sensory and motor impairment of the distal extremities. “Wet” beriberi impacts the cardiovascular system, most commonly causing dilated cardiomyopathy. Wernicke encephalopathy (WE) can present with the triad of ophthalmoplegia, ataxia, and encephalopathy. If not treated, WE can progress to Korsakoff syndrome (KS), causing anterograde and retrograde memory loss and confabulation.3
Thiamine deficiency is a laboratory diagnosis based on thiamine blood levels or erythrocyte thiamine transketolase activity (ETKA). MRI imaging shows bilateral enhancement of the mamillary bodies in 58% of patients.4 Treatment of thiamine deficiency with IV thiamine repletion should be initiated as soon as clinical suspicion arises, followed by oral supplementation.5 Wet/dry beriberi and WE improve with timely thiamine repletion, whereas KS is irreversible.
Vitamin B6 (Pyridoxine) deficiency is less understood, occurring in individuals with alcoholism, pregnancy, diabetes, and heart disease. Medications that alter vitamin B6 metabolism can also cause deficiency, such as isoniazid. Deficiency can cause irritability, depression, and confusion.6 While research has linked vitamin B6 deficiency with neuropathy, most cases documented are confounded by other nutritional deficiencies, such as thiamine. Diagnosis is made based on mean plasma pyridoxal-5-phosphate concentration. Patients typically see symptomatic improvement following oral supplementation.
Acknowledgments
Taylor Arnoff, Martin Li, Jia-Shu (Joe) Chen
Disclosures/Conflicts of Interest
The authors declare no conflicts of interest.
Funding Statement
No funding was obtained for this manuscript.
Author Contributions
All authors have reviewed the final manuscript prior to submission. All the authors have contributed significantly to the manuscript, per the International Committee of Medical Journal Editors criteria of authorship.
-
Substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work; AND
-
Drafting the work or revising it critically for important intellectual content; AND
-
Final approval of the version to be published; AND
-
Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Arkadiy Finn, MD,
Assistant Professor of Medicine, Clinician Educator,
Warren Alpert Medical School at Brown University,
Division of Hospital Medicine, The Miriam Hospital,
164 Summit Avenue, Providence, RI 02906
Tel: 401-793-2104
Email: afinn1@lifespan.org
ORCID: 0000-0002-1630-1137