Introduction
Falls and immobility in hospitalized patients have been documented as a global health problem that has negative outcomes for patients and hospitals.1–3 Patients spend approximately 83-95% of their time in bed during their hospital stay, which leads to hospital acquired patient weakness.2,4 Patients can lose 3-11% of their muscle strength and tone in as little as one day. This lack of mobility contributes to an increased risk of falls, functional decline, increased length of stay, development of pressure ulcers, pneumonia, thromboembolic disease, delirium and higher rates of discharges to skilled nursing facilities.5,6
When Centers for Medicare and Medicaid Services (CMS) announced in 2008 that hospitals would no longer receive reimbursement for care provided after a patient fall, hospitals needed to prioritize mobility and activity in order to decrease the risk of patient falls.2,4,7 It is estimated that between 700,000 – 1 million hospitalized patients have fallen each year. These falls can have devastating effects on patients and hospital organizations. Falls can result in head injuries, fractures, and death, resulting in a cost over $30,000 per patient fall.7,8 Various programs to aid in the prevention of falls, including the use of chair/bed alarms, one-to-one and remote observation have been largely unsuccessful.7 These programs have not decreased the occurrence of falls; they were found to increase nursing stress, cause alarm fatigue, fear of litigation by nursing staff, and higher healthcare costs and financial penalties.8 Fear of a patient falling while hospitalized has led to the restriction of patient’s mobility which causes loss of strength and independence with long term consequences.9
Increased time, energy and resources are being dedicated to problem solving how to decrease hospital acquired harms, with special consideration for falls. Within our organization many quality improvement projects have been proposed to remedy the frequency at which patient falls occur while admitted. A quality initiative, referred to as IMPACT (Improved Mobility Promotion through Activity, Communication and Training) was implemented by a team of occupational and physical therapists, a registered nurse and a physician with the main objective of preventing hospital acquired harms including falls, with the focus to maintain patient’s functional abilities to return home. The team utilized the Johns Hopkins AMP program as a model when developing the IMPACT initiative. AMP is an organized, standardized, interdisciplinary quality improvement program designed to increase patients’ mobility and activity levels by identifying and removing barriers to patient mobility, improving team communication and providing education. Through published research, AMP has demonstrated decreased length of stay, decreased hospital acquired harms and demonstrated that initiating a mobility promotion program does not increase fall rates.2,6
A challenge in implementing IMPACT has been the concern that increasing patient mobility will increase the occurrences of inpatient falls. That has been counter to our experience, so we evaluated this concern with our program. A participatory action research approach was used, by reflecting on our lived experiences, implementing the intervention and reviewing hospital level data on falls and patient mobility scores. If there are fewer falls when patients have greater mobility scores, this may be evidence that increasing patient mobility puts patients at less risk of falling.
Methods
To better understand the successes and difficulties in implementing this quality improvement initiative, we used a participatory action research framework. Using this approach emphasized the project leaders as active participants in the quality improvement initiative, administrating aspects of the intervention while evaluating it based on personal lived experiences. This research framework proved important as the COVID-19 pandemic interrupted our planned quantitative evaluation of changes attributable to the quality improvement initiative. While we still considered the quantitative analysis to inform our conclusions, our lived experiences working with these patients were insightful, aware of the multifaceted implications of the pandemic on patient health and willingness to be mobile. This activity does not meet the definition of research and therefore did not require IRB approval.
Sample
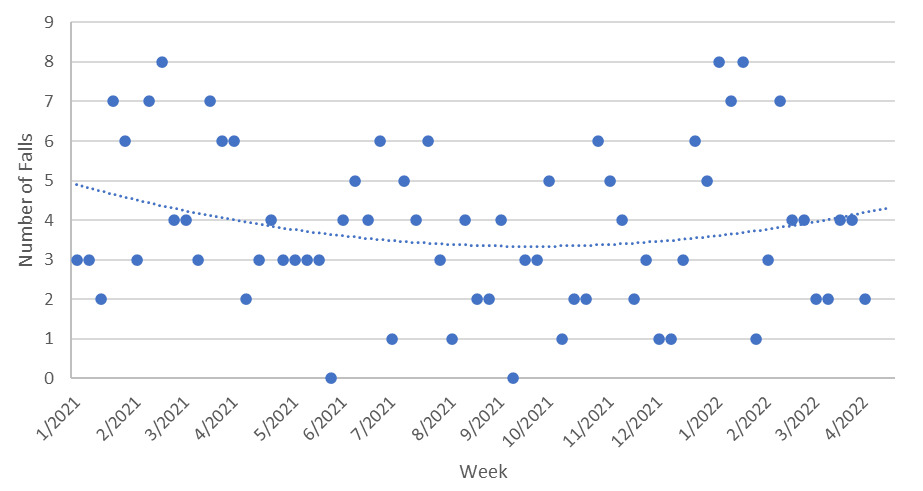
For the quantitative analysis, we included patients admitted to a 247-bed acute care hospital (Providence, RI) from January of 2021 to March of 2022. The facility is a urban nonprofit academic medical center. During this timeframe a total of 28,075 patients were discharged from this hospital and included in this analysis. Data regarding monthly hospital fall rates was obtained from the National Database of Nursing Quality Indicators (NDNQI) database. The John Hopkins-Highest Level of Mobility (JH-HLM) scale (Figure 1) was used to collect patients’ daily mobility levels. The JH-HLM is documented by nursing staff at each shift and rehabilitation staff at each visit. A report is run once weekly, pulling the highest JH-HLM of each patient admitted on that calendar day. These data points are averaged as the estimated weekly level of mobility.
Many patients presented during this time frame with moderate to high levels of mobility and were able to remain in the hospital without a decline in mobility or fall occurrence. Functional mobility was measured by the Activity Measure for Post-Acute Care (AM-PAC) Inpatient Basic Mobility Short Form 6-Clicks. On this scale a total raw score ranges from 6-24 (higher score is better). In the setting of an acute care hospital in 2021, mobility restrictions were an unfortunate consequence of the COVID-19 pandemic. With a goal of reducing the spread of illness, patients that tested positive for the SARS-CoV2 virus were placed in isolation with restrictions of leaving their rooms, unless medically required.
Analysis Plan
Vector autoregressive modeling was used to compare the weekly changes in falls and JH-HLM scores. In this approach, the average number of both events are jointly estimated as a function of time. Additionally, the correlation over time is estimated between the falls and JH-HLM scores while accounting for the average changes over time. Lastly, the association is estimated between the previous week’s and the current week’s number of falls and JH-HLM scores. The association allows for the precise decomposition of sources of change over time to identify whether any observed changes are the accumulation of random variation, average increases and decreases, or cross sectional correlation. Interprofessional staff were concerned that increased patient mobility placed patients at a greater risk for falls. If there were evidence of this, then the cross sectional correlation would be positive between falls and JH-HLM scores when accounting for all other time related trends. The trend was tested analytically.
Results
Lived Experience
A primary challenge we experienced in implementing this intervention was the concern that increasing mobility would put patients at greater risk of falling. In our experience working with patients, we felt a greater concern for hospital acquired harm due to immobility. For example, one patient we worked with was admitted with congestive heart failure and was assessed to have an admission AM-PAC Basic Mobility score of 12 and a JH-HLM score of 7. During the 2-day length of stay (LOS), the AM-PAC Basic Mobility score improved to 18 and the JH-HLM score of 7 was maintained. The patient did not fall, improved in mobility independence and was able to return home.
What we found to be of particular concern was how falls were likely to occur as patients became weaker, sicker, often resting longer in bed. A patient with a 16-day LOS experienced a fall toward the end of the hospitalization. Initially this patient admitted with shortness of breath and diarrhea, was assessed at an 18 AM-PAC Basic Mobility and a JH-HLM of 6. After the lengthy hospital stay and the fall event, the patient was assessed as a 15 AM-PAC Basic Mobility and JH-HLM of 3 at discharge going to a skilled nursing facility (SNF). A second example involves a patient admitted with leg pain with a LOS of 7 days. Assessment of the patient yielded an AM-PAC Basic Mobility score of 12 and JH-HLM of 3 upon admission, experienced a fall event and was then discharged to SNF when medically stable with an AM-PAC Basic Mobility of 9 and JH-HLM of 2.
These cases demonstrate how patients in poor health condition, exposed to prolonged inactivity, lead to decline in mobility over time. To address this, a critical aspect of our initiative became educating hospital staff about the ways in which patients can improve activity and mobility levels and the risks of inactivity. While increasing mobility may mean more opportunities to fall, a lack of mobility can facilitate further deterioration of physical abilities.
The COVID-19 pandemic restrictions presented many challenges. Although there are many situations in which the COVID-19 virus caused functional and medical decline, mobility promotion along with appropriate medical care was seen to promote recovery and discharge to home. A patient admitted for SARS-CoV2 infection had an initial AM-PAC Mobility score of 13 and JH-HLM of 3. After an 8-day LOS they returned home with an improved AM-PAC Basic Mobility score of 19 and JH-HLM of 6.
Quantitative Analysis
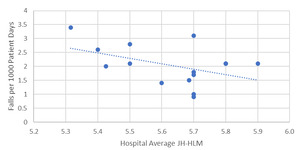
Figure 2 plots the number of falls per week over time, and Figure 3 the average JH-HLM scores. Visual examination demonstrated clear curvilinear trends, so we allowed for a quadratic trend over time. When accounting for average trends over time and stochastic association, there was a decrease in JH-HLM scores on average over time = -0.15, p = 0.0548). This may be attributable to increased restrictions on patient mobility during the COVID-19 pandemic; or a week of unexpectedly low mobility scores during November 2021. Falls demonstrated a quadratic trend = 0.29, p = 0.0430). The remaining cross sectional correlation between the two trends was not statistically significant = 0.10, p = 0.1434). While lack of evidence of an association is not necessarily evidence of a null association, this is consistent with our hypothesis that increasing patient mobility would not demonstrate increased risk of falling. Additionally, when patients had the best mobility, falls were lowest, a significant difference in quadratic trends = 0.43, p = 0.0430). This is further demonstrated in Figure 4 which plots the falls per 1,000 patient days over the hospital average JH-HLM.
Discussion
IMPACT was implemented by a multidisciplinary clinical team to prevent hospital acquired harms caused by immobility. During the time frame of January 2021 to March 2022, data was collected that demonstrated a relationship between fall occurrence and mobility levels. When tracking fall and mobility data over time, we demonstrate increased mobility does not cause an increase in falls. When mobility scores increased, during that same time frame, falls decreased.
We sought to evaluate the risks of an unfounded “cultural” belief that increased patient mobility led to increased falls. We found this to be a top concern among providers, however there appeared to be a lack of awareness about the risk inactivity poses to longer term mobility. It has also been noted that as patients are more deconditioned, their likelihood of requiring a post-acute inpatient rehab stay increases significantly. There are multiple harms that can be prevented by frequently mobilizing patients in the hospital, it only makes sense that with less deconditioning and fewer immobility associated complications, mobile patients fall less often.3,10,11 This supports the main conclusions of our analysis.
There is strong evidence highlighting that there is little to no benefit to bedrest in most cases, and that there are multiple harms that patients incur with prolonged periods of bedrest including blood clots, deconditioning, contractures, increased risk for or worsening of pneumonia, edema, and delirium.2–6,10 These are examples of medical and cognitive declines that lead to inpatient falls. Inpatient falls can also result from inaccurate fall risk assessment interpretations, breakdowns within communication, fear avoidance culture, inopportune environment for safe mobility, and side effects of medications used during hospitalization.,12,13 fear of patients falling has been a barrier preventing staff from mobilizing patients.8,14 In a randomized control trial, a group of hospitalized patients receiving usual care were compared to a group enrolled in a mobility program. This study looked at many quality outcomes including falls and found that falls were more likely to occur in the usual care group than the mobility program group, enhancing the argument for mobility to be used as an intervention to reduce hospital falls.11 Our results are consistent with these outcomes.
One of the limitations of this quality improvement study is the unknown effects of the COVID-19 pandemic. Staff shortages and turnover that occurred during the pandemic brought unique challenges to hospital wide initiatives with complex competing priorities for patient care along with decreased opportunities for education.14 In our lived experience we found ongoing clinical staff education is critical in order to minimize immobility harm. Acquisition of data was another limitation. Averages of patient mobility were taken from a weekly sampling audit. Further investment of daily auditing would potentially lend strength to the precision of estimated association. Access to daily data would allow for further research to determine the effects of staffing ratios, patient census and acuity as well as other quality improvement initiatives occurring simultaneously. This is especially important because the nonsignificant association is not necessarily evidence of a null association. While there were limitations in data collection that complicated interpretation of quantitative results, we found that when mobility scores were highest, falls were lowest and there was minimal cross-sectional correlation between the two.
Moving forward, IMPACT will be implemented across our multi-hospital organization which will allow us to determine if these results generalize to a broader patient population. Hoyer et al. noted in a recent paper in 2022 that to promote increased activity and mobility, it is important to set a daily mobility goal to patients.3,15 In our analysis, patients scores ranged mostly between JH-HLM of 5-6 (standing for 1 minute; 5; or taking 10 steps; 6). If we were to increase average mobility scores to baseline ambulation levels (at least a 7: walking 25 ft or more if not an 8: walking 250 ft or more), we hypothesize a stronger inverse relationship between falls and mobility. In a meta-analysis of hospital falls, education was the most effective strategy for reducing the rate and risk of hospital falls.14 This highlights the importance of reinforcing education at select intervals moving forward. Improvements in data collection to include daily data as well as goal achievement will strengthen the evidence in trends that occur as mobility increases. Our IMPACT team is a dynamic group that is frequently making changes, increasing education and providing multi modal learning opportunities for the interdisciplinary staff to promote increased activity and mobility in our hospitalized patients, and enhance staff confidence in safe mobility practices.
Conclusion
The results of this quality initiative showed a relationship between hospital mobility and falls. During this timeframe when hospital-wide mobility levels were higher, falls per 1000 patient days were lower. With strong interdisciplinary education to increase awareness of immobility harms, culture around fall prevention will no longer support limiting mobility. The growing body of evidence that links falls and immobility support the continuation of mobility promotion quality improvement initiatives. We found frequent mobilization helped to prevent these harms.
Conflicts of Interest
The authors declare no conflicts of interest.
Funding Statement
No funding was obtained for this manuscript.
Author Contributions
All authors have reviewed the final manuscript prior to submission. All the authors have contributed significantly to the manuscript, per the International Committee of Medical Journal Editors criteria of authorship.
-
Substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work; AND
-
Drafting the work or revising it critically for important intellectual content; AND
-
Final approval of the version to be published; AND
-
Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Acknowledgments
None.
Corresponding Author
Heidi Kissane, PT, DPT
Department of Rehabilitation Services
The Miriam Hospital
164 Summit Avenue, Providence, RI, USA
Tel: 401-793-2500
Fax: 401- 793-7482
_scale.png)

_scale.png)