Background
Hospitals world-wide serve as a catch-all mechanism for patients with a broad range of diseases. Hospital-based providers, in the emergency department and inpatient settings, are faced with rapid identification and triage of transmissible infectious diseases that pose a safety risk to other hospitalized patients and hospital staff. Although the previous three decades have seen a rise in hospital-based infection prevention programs in addition to expanding knowledge about prevention methods such as hand hygiene and appropriate isolation, knowledge amongst providers appears to be variable.1 Outbreaks of nosocomial infections are common world-wide suggesting that there is much progress to be made in improving patient safety in this domain.2–4 We review six commonly presenting conditions associated with high likelihood of nosocomial spread and suggest strategies for effective infection prevention.
Scabies and Crusted (Norwegian) Scabies
Scabies, a condition caused by the mite, Sarcoptes scabiei varietas hominis, is a cutaneous disease characterized by a pruritic rash often affecting immunocompromised, malnourished and immobilized individuals and inadequate self-hygiene.5 The mites reproduce by digging burrows and laying eggs in the stratum corneum of human skin. Cutaneous manifestations include papular, papulo-vesicular or nodular rashes affecting the trunk and extremities.6 Crusted scabies, also known as crusted (Norwegian) scabies, an extreme form of scabies, characterized by uncontrolled mite replication and extensive crusting (hyperkeratosis) of the hands, feet, elbows and neck, can occur in individuals who have chronic diseases, are immunosuppressed, have compromised skin functionality, or have impaired physical capability.7,8 Appearance of scabies in the elderly adult may be atypical; 51% of patients were asymptomatic and 25% lacked evidence of cutaneous burrows.9 Failure to find mites in the skin does not rule out infection.10 The risk of spread, particularly in the hospital, is very high as patients who are not able to mount an immune response are more likely to be impacted. Mites can survive outside the human body for 24-48 hours at room temperature and relatively humid air.5 Infection may be transmitted by a single mite. Missed and delayed diagnosis leads to nosocomial spread with outbreaks lasting three months on average.11,12
An identified outbreak should be brought to the attention of the local health department and patients with an active scabies infestation should be immediately isolated to reduce spread.13 The speed of response and intervention dramatically decreases spread. Topical permethrin and oral ivermectin are used to treat scabies in affected cases thereby also limiting spread.14 Staff and visitors who interact with infected patients should follow strict contact precautions and always wear appropriate protective equipment including gloves, a gown, and shoe covers. The number of people that interact with the patient should be limited to reduce spread. Thorough hand sanitation should be done before and after contact. Similarly to crusted scabies, all persons who interact with patients with non-crusted scabies should avoid direct skin-to-skin contact and wear appropriate PPE including gloves. Thorough hand sanitation should be performed before and after contact.
For both crusted and non-crusted scabies, used linens should be washed and dried at a temperature of at least 50℃ (122℉).15 All persons who have come in contact with the patient, including visitors and family members prior to known infestation, should be identified and treated immediately. Though thorough decontamination measures are not required for non-crusted scabies once patients have been discharged, the process is necessary for crusted scabies.
Tuberculosis
Tuberculosis (TB) is an infectious disease caused by the bacterium Mycobacterium tuberculosis which primarily spreads through airborne particles produced by infected individuals when they speak, cough, sneeze, or sing. Though TB cases have gradually declined in the US since 1993, it remains a significant cause of morbidity and mortality worldwide.16,17 The majority of TB cases in the US are in foreign born individuals from endemic areas of the world. TB is believed to be primarily transmitted indoors via airborne particles and outbreaks have occurred in hospitals and other congregate settings.18 Shared patient rooms, immunocompromised state of hospitalized patients, and delayed isolation may lead to transmission and increased risk of severe disease. The role of the clinician is rapid recognition and isolation of the patient with suspected and/or confirmed pulmonary TB. Factors associated with delayed isolation include older age, comorbid malignancy, admission department other than Infectious Diseases and Pulmonary, and the absence of the diagnosis of active TB on the admission chest radiograph.18 Conditions such as malignancy and autoimmune disease are also associated with delayed diagnosis of TB.19 Clinicians must carefully consider respiratory and constitutional symptoms (cough, weight loss, fatigue) and abnormal chest radiograph findings in patients possessing risk factors for TB including exposure to an infected person, human immunodeficiency virus (HIV) infection, medically underserved populations, immigration from a geographic area with high TB incidence, history of incarceration, and others (Table 1).20
Hospital inpatient interventions are based on a three-level hierarchy of control measures: administrative measures, environmental controls, and use of protective equipment (PPE).21
-
Developing infection prevention policies, procedures, and guidelines that align with established standards is crucial in preventing TB infections.22
-
Isolation of patients in airborne infection isolation rooms and management of ventilation and adequate air exchange in the hospital are important in maintaining diligence when considering environmental controls.23
-
Protective equipment includes N95 masks which should be worn by health workers when entering room of patients with suspected or confirmed TB.
Effective treatment of TB rapidly leads to decreased infectiousness.
Respiratory Viruses
Infection caused by respiratory viruses (RV) can cause upper and lower respiratory infections (URI), with a clinical presentation characterized by myalgias, low-grade fever, nasal congestion, and rhinorrhea.24 URI is benign, is the most common infection worldwide, and is known as the common cold. Over 200 viruses have been found to cause URI. Among them are rhinoviruses, metapneumoviruses, parainfluenza, and strains of adenovirus and coronavirus.25 Influenza and respiratory syncytial virus are RVs that cause illnesses more severe than URI that can be potentially deadly in infants and individuals with comorbidities.26 Hospital acquired influenza when compared to community acquired influenza is associated with a higher rate of ICU admission, need for mechanical ventilation and death.27,28 Furthermore, RVs can be the cause of pandemics, such as the coronavirus SARS-CoV-2, which causes COVID-19 and is more severe than circulating RVs and possibly lethal in healthy individuals. RV transmission is usually seasonal, with higher transmission in cooler months.25 Rhinovirus is the most common pathogen in adults and is the leading cause of community acquired pneumonia in hospitalized patients.29,30
Despite the vast number of respiratory viruses, infection mitigation strategies between them are similar. The cornerstone in preventing RV transmission is appropriate masking and hand hygiene, namely washing hands with soap and water for 20 seconds or using approved alcohol-based hand sanitizer after each encounter with a patient. This has been repeatedly shown to decrease RV transmission both in the community and in hospital settings.26,31 The other hallmark in RV mitigation is source control with surgical grade face masks, which prevent spread of respiratory droplets (those >5µm) from individuals with suspected RV.32 Healthcare workers who interact with suspected or confirmed RV patients should wear surgical masks, don gowns and gloves, and wear eye protection.26 N95 respirators should be used for protection from COVID-19. In periods where RV transmission is high, universal masking by all individuals regardless of symptom status might be recommended by local or CDC guidelines. For patients with confirmed or suspected URI, isolation protocols are often employed. Lastly, a yearly recombinant vaccination and mRNA vaccination exist for influenza and COVID-19, and these have been shown to effectively prevent some infections and markedly reduce the severity of infection with these viruses.26
Varicella Zoster Virus
Varicella Zoster Virus (VZV) is a highly contagious pathogen that is transmitted via respiratory droplets and is a well-documented source of nosocomial infection. Primary VZV infections result in a diffuse, generally self-limiting, vesicular rash known as “chickenpox”.33 VZV then has the ability to lay dormant and cause endogenous secondary infections decades later, which is known as “shingles”.33 Given the potential for serious complications in neonates and immunocompromised persons, several measures must be put in place to limit the spread of VZV in the hospital setting. The CDC provides a framework for preventing transmission from two perspectives: patient isolation and healthcare personnel prophylaxis.34 With respect to patient isolation, any patient who is admitted to the hospital and is suspected, or confirmed, to have a primary varicella or disseminated VZV infection should be placed on contact and airborne precautions. These precautions should consist of alcohol-based hand hygiene after each patient contact in combination with the donning of a gown, gloves, eye protection, and the use of a certified N95 respirator by personnel in patient care areas. Patients should be kept on these precautions until the lesions have dried and crusted over.35,36 With respect to protection of hospital personnel, the CDC recommends all personnel be adequately immunized to VZV at the time of initial employment; confirmation of sufficient immunization status can be achieved through written documentation show the receipt of the two-dose varicella vaccine series, laboratory evidence of disease-induced immunity, or written documentation of prior varicella diagnosis by a healthcare provider.36
Clostridioides difficile
Clostridioides difficile (formerly known as Clostridium difficile), a spore forming gram-positive anaerobic bacillus, is the leading cause of nosocomial diarrheal illness and is an important focus with respect to institutional infection prevention.37,38 In 2014, C. difficile was the number one organism responsible for health care associated infections.39 Per the current CDC recommendations, any patient with a suspected or confirmed Clostridioides difficile infection (CDI) should be placed on isolation and contact precautions.37 These precautions should consist of, when feasible, placing patients in single-patient rooms, having dedicated patient-care equipment, and ensuring proper contact precautions are adhered to when the patient is transported throughout the facility; all hospital employees who are entering a patient’s room should don the appropriate personal protective equipment, which would consist of a high-quality gowns and gloves at a minimum.37,38 Contact precautions should ideally be in place for at least 48 hours after the resolution of diarrheal symptoms, but can be left in place up to the duration of the hospitalization due to Clostridioides difficile’s prolonged spore shedding time.40 In addition to these measures, adequate hand hygiene, should be employed by all hospital staff members and the patient after each encounter.41 Another essential policy that should be enacted in prevention of CDI is appropriate environmental cleaning procedures; the CDC recommends all CDI patient rooms and equipment undergo a daily cleaning, in addition to a terminal cleaning at the end of the patient’s stay, with a Clostridioides difficile sporicidal agent (EPA List K agents).42 Lastly, healthcare providers should make concerted efforts to practice effective antibiotic stewardship by limiting the use and duration of antibiotics that increase the risk of CDI, such as fluoroquinolones, carbapenems, and 3rd/4th generation cephalosporins.42
Syphilis
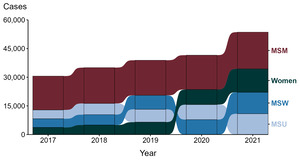
The transmission of syphilis is commonly associated with sexual intercourse but can also occur through other means. In the past, when syphilis was more prevalent, there were reports of occupational infection, where the infectious agent was acquired by a healthcare provider during the provision of a medical service. Prior to the standard practice of using gloves by healthcare providers, there were reports of extragenital syphilitic lesions on the fingers and in the noses of physicians.43–45 A study by Epstein et al. found a report of 51 cases of extragenital chancres in physicians; thirty-five of these lesions occurred on the fingers, six inside the nose, one on an eyelid and one on an arm.43 Routine examinations of patients was the most common means of infection, and not wearing gloves was a recurrent reported reason as to how the transmission occurred. Examination of patients, deliveries, pelvic examinations, needle punctures and tonsillectomies seemed to be the most dangerous procedures.43 Because patients have spirochetemia, syphilis is a blood borne pathogen. Transmission occurs when there is contact with open wet lesions (chancre, mucous patches, condyloma lata, lues maligna).44 Dry and intact lesions of syphilis are non-contagious. Given that occupational infections of syphilis have occurred, it is important to use precautions when treating patients with syphilis in the inpatient setting. The CDC recommends that healthcare providers caring for patients with syphilis infection use standard precautions.35 This includes any or all the following: hand hygiene, the use of gloves, gown, mask, eye protection, or face shield, depending on the anticipated exposure; and safe injection practices. Also, equipment or items in the patient environment likely to have been contaminated with infectious body fluids must be handled in a manner to prevent transmission of infectious agents (e.g., wear gloves for direct contact, contain heavily soiled equipment, properly clean and disinfect or sterilize reusable equipment before use on another patient).35 The number of syphilis cases in the United States has risen over the past several years (Figure 1).
Conclusion
Infection prevention in the hospital is of paramount importance to patient safety as well as the safety of healthcare workers and visitors. Hospital-based providers must maintain a high level of vigilance for common, highly transmissible conditions and prevent transmission throughout the hospital. Scabies, tuberculosis, respiratory viruses, VZV, CDI, and syphilis are only some of the conditions at risk of nosocomial spread. The task of inpatient infection prevention is shared by providers, nurses, infection prevention teams, environmental services and others who must coordinate efforts in order to improve patient safety and outcomes.
Author Contributions
All authors have reviewed the final manuscript prior to submission. All the authors have contributed significantly to the manuscript, per the International Committee of Medical Journal Editors criteria of authorship.
-
Substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work; AND
-
Drafting the work or revising it critically for important intellectual content; AND
-
Final approval of the version to be published; AND
-
Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Disclosures/Conflicts of Interest
The authors declare no conflicts of interest.
Funding Statement
No funding was obtained for this manuscript.