INTRODUCTION
Biliary stricture is a narrowing of the biliary tree, and often presents with features of obstructive jaundice. It is frequently associated with pancreaticobiliary neoplasms, with pancreatic cancer and cholangiocarcinoma being the most important causes.1 However, up to 30% of biliary strictures are benign, and often result from iatrogenic injury, most commonly with laparoscopic cholecystectomy.2 Other etiologies of benign strictures include, primary sclerosing cholangitis, recurrent pyogenic cholangitis, acquired immune deficiency syndrome (AIDS) associated cholangiopathy, and chemotherapy-induced sclerosing cholangitis.3 These and others have been listed in the Table. Determining the malignant nature of a stricture is critical as benign biliary strictures (BBS) are typically managed endoscopically while surgery is often reserved for malignant strictures.4 History and clinical presentation can provide indications that may be helpful in determining the pretest probability of malignancy and guide further work up.3 A combination of computed tomography scan (CT), magnetic resonance cholangiopancreatography (MRCP), and endoscopic ultrasound (EUS) are currently used to identify malignant strictures, with diagnostic accuracy ranging from 60-80%.5 A recent review of literature shows that one in four patients undergoing surgical resection for suspected malignant biliary stricture will ultimately prove to have benign etiology.6–8 With rare exceptions, the etiology of biliary strictures cannot be confirmed on the basis of non-invasive testing. This is more difficult when the stricture is not associated with a mass. Although a unified definition is lacking, the term ‘indeterminate biliary stricture’ has been used to describe strictures in which the malignant nature cannot be elucidated even after non-invasive testing and an ERCP have been performed.4 Novel ancillary techniques have emerged which help improve diagnostic accuracy in such cases. One such technique, cholangioscopy, allows for direct visualization and tissue acquisition of the indeterminate biliary strictures. We present a case of painless jaundice where cholangioscopy played a crucial role in making the diagnosis.
CASE DESCRIPTION
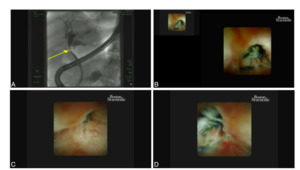
A 76-year-old man with a past medical history of hypertension and diabetes mellitus, and a past surgical history of a laparoscopic cholecystectomy ten years prior to presentation presented to hospital for one week of jaundice, darkening of urine, and pruritus. He denied any weight loss, abdominal pain, nausea, or vomiting. Physical exam was notable for icterus, and the abdomen was soft and non-tender without any palpable masses. Laboratory evaluation was significant for a total bilirubin of 14.8 mg/dL (0.1 to 1.2mg/dL), direct bilirubin of 7.6 mg/dL (0.3 mg/dL) , AST 40 U/L (8 to 33 U/L), ALT 56 U/L (4 to 36 U/L), and alkaline phosphatase of 128 U/L ( 44 to 147 U/L). MRCP was obtained, which showed a poorly defined soft tissue lesion at the common hepatic duct (CHD) with intrahepatic ductal (IHD) dilation. The patient was referred for EUS and endoscopic retrograde cholangiopancreatography (ERCP) for further evaluation. EUS revealed IHD dilation and a benign appearing porta hepatis lymph node without endosonographic evidence of pancreatic mass or cysts. The lymph node at the porta hepatis was sampled using fine needle aspiration (FNA). ERCP was then performed, revealing a single stenosis at the level of the CHD with upstream dilation suggestive of malignancy, shown in Figure 1, Image A. Cholangioscopy was performed, which showed an inflammatory-appearing stenosis of the CHD with embedded suture material (Figure 1, Images. B, C &D). The stenosis was biopsied using mini forceps and subsequently dilated with a balloon dilator. An 8.5 Fr x 10 cm Advantix™ (Boston Scientific, Marlborough, MA) plastic biliary stent was placed with subsequent improvement in the patient’s hepatic function. FNA cytology and final pathology of the CHD stricture were both negative for malignancy.
The patient made an uneventful and complete recovery and was seen in the clinic 4 weeks after the procedure.
DISCUSSION
Non-invasive imaging modalities such as CT and MRCP, are useful in determining presence and location of biliary strictures, but a significant proportion of these strictures do not have an associated mass lesion.9,10 Invasive imaging methods are required to directly visualize and obtain tissue as tissue acquisition remains the gold standard for diagnosis.11 Tissue acquisition techniques currently in widespread use include, transpapillary fluoroscopy-guided biopsy and brush cytology during ERCP. A proposed flowchart for the diagnosis of biliary strictures is indicated in Figure 2. These techniques, however, have decreased diagnostic sensitivity.4 It is not uncommon to encounter situations where the etiology of stricture cannot be determined with imaging or tissue diagnosis alone, and this is likely due to the relative acellularity and desmoplastic reaction surrounding malignant biliary strictures. Indeterminate biliary strictures pose a diagnostic dilemma as up to 70% of these strictures are malignant.12 In such cases where the suspicion of malignancy is high, cholangioscopy is recommended during the index ERCP.4 With improvement in the image resolution and increase in the availability, cholangioscopy has become an important tool for evaluation of indeterminate strictures. Cholangioscopy allows for detailed visual inspection of strictures and facilitates targeted biopsies under direct visualization. Both direct visualization and targeted biopsy via cholangioscopy are helpful in diagnosis, and the visual impression adds sensitivity to the biopsy which is inherently specific.
There is a lack of consensus on the position of cholangioscopy in the diagnostic algorithm of biliary strictures. The pretest probability of malignancy can guide in timing of performing a cholangioscopy. The pretest probability of identifying a malignant biliary stricture depends on clinical features that may present at the time of the initial presentation. The antecedent history of cholecystitis, pancreatitis, or biliary manipulation as well as the lack of disease progression over any 6-month period is highly suggestive of benign etiology. Cholangioscopic and other imaging characteristics that include tumor vessels, papillary projection, nodular or polypoid mass, and infiltrative lesions are frequently associated with malignancy. Using these metrics as well as careful history and examination looking for other elements of the history such as history of exposure, significant tobacco or alcohol use, loss of more than 10% of body weight in an unintentional manner, as well as family history of cancers can provide a framework to gauge the pretest probability of any given biliary stricture being malignant. Although guidelines have recently been proposed for the use of cholangioscopy to diagnose indeterminate biliary strictures, no scoring systems have currently been shown to reliably predict malignancy in a biliary stricture without pathological confirmation.4
In this case, due to high concern for malignancy with common hepatic duct stenosis and proximal dilation, a negative brush cytology alone may not have been sufficient to rule out cholangiocarcinoma, as the sensitivity of brush cytology in evaluating malignant hilar strictures has been reported as low as 41.4%.13 While this is not a new technique, cholangioscopy and brush cytology have been directly compared in their ability to identify malignancy. A prospective, randomized study comparing cholangioscopy-guided biopsy to brush cytology demonstrated that cholangioscopy-guided biopsy was not only significantly more sensitive in detecting cholangiocarcinoma in indeterminate biliary strictures, but also was significantly more accurate.14 Visual characteristics seen during cholangioscopy can also help differentiate benign and malignant biliary strictures with high accuracy.15 In this case, the pretest probability of malignancy was high given the age and symptoms of obstructive jaundice. However, given the history of cholecystectomy, a benign postoperative stricture was well within the realm of the differential diagnoses.
Cholangioscopic assessment and biopsy allowed appropriate identification of underlying pathology, ruled out malignancy and prevented unnecessary surgery. Our approach also reduced the need to perform multiple procedures. This patient likely sustained a bile duct injury during his prior cholecystectomy, which was repaired with a suture, leading to an inflammatory stricture, and symptoms of obstructive jaundice years later.
Iatrogenic strictures make up about 30% of all benign strictures, with cholecystectomy being one of the most important associated risk factors.3 The rates of bile duct injury are higher with laparoscopic surgeries. The incidence of iatrogenic bile duct injury following laparoscopic cholecystectomy has been reported to be as high as 3%.16 The incidence of biliary strictures after laparoscopic cholecystectomy is approximately 0.5%, caused by direct surgical bile-duct injury due to misidentification of biliary duct for cystic duct.17 Obtaining an intraoperative cholangiogram, has shown to decrease incidence of such injuries.18,19 Repair of bile duct injuries may result in stricture formation, with symptoms, sometime, occurring several years after repair. There have also been reports of bile duct stone formation with polypropylene and other permanent suture.20 With advancement in ERCP, endoscopic dilatation followed by placement of multiple plastic stents has taken over conventional surgical interventions for management of benign strictures. With the majority of indeterminate biliary structures being malignant, our case is an example of a benign stricture, where clinical history helped unveil important information regarding an alternate etiology.
A significant limitation of cholangioscopy remains the inability to evaluate extrinsic sources of biliary compression, as well as distal biliary lesions.20 There is also currently a lack of standardization in the classification of observations from cholangioscopy. Other significant limitations include small specimen size as well as the increased risk of adverse events including a higher rate of cholangitis necessitating drainage, and periprocedural antibiotic coverage. Finally, the increased procedural time, and cost of performing this routinely has not been calculated from the patients’ as well as health care systems perspectives. Newer emerging technologies for biliary imaging include confocal laser endomicroscopy, autofluorescence imaging, and optical coherence tomography. All of these are designed to offer greater resolution, higher image clarity and a virtual biopsy to increase the sensitivity of the actual final pathological specimen obtained.21
This report highlights the importance of definitive diagnosis using cholangioscopy with biopsy, in cases where the pretest probability of malignancy may be high, thus, preventing the unnecessary morbidity of major abdominal surgery.
Corresponding Author
Aarushi Sudan, MD
Jacobi Medical Center, 1400 Pelham Parkway S, Bronx, New York 10461
Phone: 516-871-7147
Email: aarushi.sudan@gmail.com
Conflicts of Interest
The authors declare no conflicts of interest.
Funding Statement
No funding was obtained for this manuscript.
Author Contributions
All authors have reviewed the final manuscript prior to submission. All the authors have contributed significantly to the manuscript, per the International Committee of Medical Journal Editors criteria of authorship.
-
Substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work; AND
-
Drafting the work or revising it critically for important intellectual content; AND
-
Final approval of the version to be published; AND
-
Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Acknowledgments
None.